The intricate dance between stress and human biology has captivated scientists for decades, revealing a complex interplay that leaves lasting marks on our cellular machinery. Recent research illuminates how chronic stress orchestrates a symphony of biological changes, from the microscopic fraying of chromosome caps to chemical alterations that rewrite our genetic playbook. These discoveries are reshaping our understanding of stress not as a fleeting psychological state, but as a biological sculptor that chisels its signature across our very DNA.
Telomeres: The Biological Hourglass of Stress
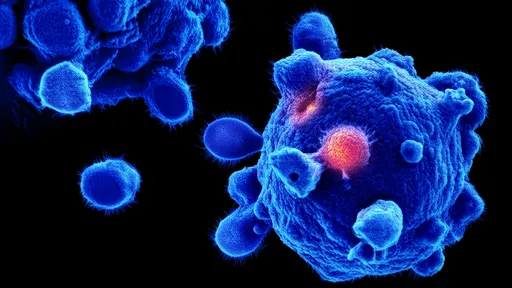
At the chromosome's tips, telomeres serve as protective caps much like plastic tips on shoelaces. These repetitive DNA sequences naturally shorten with each cell division, but stress dramatically accelerates their erosion. The enzyme telomerase normally compensates for this wear, yet chronic stress suppresses its activity while simultaneously increasing oxidative damage. This double assault transforms telomeres into a biological ledger, recording years of stress exposure in their dwindling length.
Studies of caregivers and trauma survivors reveal telomeres up to a decade older than their chronological age would predict. The stress hormone cortisol emerges as a key culprit, its prolonged elevation creating cellular conditions ripe for telomere degradation. Remarkably, mindfulness practices appear to buffer this effect, with long-term meditators maintaining telomere lengths comparable to unstressed controls. This finding suggests our biological age may be more malleable than previously imagined.
Epigenetics: Stress's Molecular Graffiti
Beyond telomeres, stress leaves its mark through epigenetic modifications - chemical tags that decorate DNA and histones without altering the genetic code itself. These molecular annotations act like volume knobs for genes, amplifying or silencing their expression in response to environmental cues. Glucocorticoid receptors, which mediate stress responses, show particular epigenetic sensitivity, creating feedback loops that can perpetuate stress reactivity across the lifespan.
The groundbreaking Bucharest Early Intervention Project demonstrated how early-life stress alters DNA methylation patterns in genes regulating neural development and immune function. These changes persisted years after children were removed from neglectful environments, illustrating epigenetics' role as a molecular memory keeper. Animal models reveal similar mechanisms, where maternal care quality sets epigenetic programs affecting stress responses in offspring - a haunting example of biology echoing experience across generations.
The Stress-Gut-Brain Axis: A Triangular Conversation
Emerging research spotlights the gut microbiome as both mediator and target of stress biology. Chronic stress reshapes microbial communities, reducing diversity while favoring inflammatory species. This dysbiosis then feeds back to influence brain function through multiple pathways, including vagal nerve signaling and microbial metabolite production. Short-chain fatty acids from beneficial bacteria appear particularly important, modulating both epigenetic processes and neuroinflammation.
Fascinatingly, germ-free mice exhibit exaggerated stress responses that normalize after receiving microbiota transplants from unstressed counterparts. Human trials with psychobiotics - live organisms with mental health benefits - show promise in breaking stress's vicious cycles. These findings position the gut as a novel therapeutic target for stress-related disorders, offering approaches that complement traditional neurological interventions.
Cellular Memory: When Stress Becomes Biological Destiny
At the cellular level, stress triggers mitochondrial adaptations that can become maladaptive over time. Initially protective metabolic shifts aimed at energy conservation may harden into inefficient states resembling accelerated aging. The unfolded protein response, meant to handle stress-induced protein damage, can transition from temporary coping mechanism to chronic endoplasmic reticulum stress - a hallmark of numerous age-related diseases.
Perhaps most remarkably, stem cells appear to retain molecular memories of stress exposure that influence their differentiation potential. This cellular priming may explain why early adversity increases vulnerability to conditions like cardiovascular disease decades later. Researchers are now mapping these biological footprints, seeking points where timely intervention might redirect trajectories toward resilience rather than pathology.
Rewriting the Stress Narrative: From Damage to Dialogue
The latest science reframes stress not as an inevitable destroyer but as a biological conversation - one we can learn to modulate. Techniques like heart rate variability biofeedback train individuals to influence stress response systems consciously. Nutritional strategies targeting methylation pathways show potential for modifying stress-related epigenetic marks. Even simple interventions like controlled breathing appear to reset gene expression patterns in white blood cells within minutes.
This evolving understanding carries profound implications. By decoding stress's biological language, we move closer to personalized interventions that address not just psychological symptoms but their physical incarnations. The goal shifts from stress elimination to stress literacy - developing the capacity to navigate life's pressures without letting them etch permanently into our biology. As research continues unraveling these mechanisms, we gain not just knowledge about stress, but power over its most enduring consequences.
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025