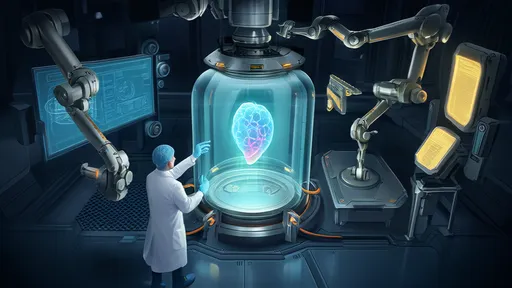
The concept of digital twins—virtual replicas of physical entities—has transcended its industrial origins and is now making waves in the biomedical field. Among the most groundbreaking applications is the development of virtual organ simulations, which promise to revolutionize medical research and drug testing. The idea of replacing or reducing human trials with these sophisticated digital models is no longer science fiction but an emerging reality. As technology advances, the ethical, scientific, and practical implications of this shift are coming into sharp focus.
At its core, a digital twin of a human organ is a highly detailed computational model that mimics the structure and function of its biological counterpart. These models are built using vast amounts of data, including medical imaging, genetic information, and real-time physiological measurements. Unlike traditional simulations, digital twins are dynamic, evolving with new data inputs to reflect changes in the organ’s state. For instance, a virtual heart model can simulate how a patient’s cardiac tissue responds to a new medication, offering insights that would otherwise require invasive procedures or lengthy clinical trials.
The potential benefits of virtual organ simulations are immense. One of the most compelling advantages is the reduction of reliance on animal and human testing. Drug development, for example, is a notoriously slow and expensive process, often fraught with ethical dilemmas. By using digital twins, researchers can predict how a drug will interact with human tissues before it ever reaches a living subject. This not only accelerates the development timeline but also minimizes risks to trial participants. Early successes in this area, such as the use of liver models to predict drug toxicity, suggest that the technology could soon become a standard tool in pharmaceutical research.
However, the road to widespread adoption is not without obstacles. Creating accurate digital twins requires an unprecedented level of data granularity. Every individual’s biology is unique, and capturing this variability in a virtual model is a monumental challenge. Current models often rely on generalized data, which may not account for rare genetic mutations or atypical physiological responses. Critics argue that until these models can be personalized with high precision, their utility in replacing human trials will remain limited. Moreover, the computational power needed to run these simulations at scale is staggering, raising questions about accessibility and cost.
Ethical considerations also loom large. While reducing human and animal testing is a laudable goal, the question of how much trust we can place in digital simulations remains unresolved. Regulatory agencies like the FDA and EMA are still grappling with how to validate these models for clinical use. If a virtual organ fails to predict a drug’s adverse effects, the consequences could be dire. Striking the right balance between innovation and safety will be crucial as the technology matures.
Despite these challenges, the momentum behind virtual organ simulations is undeniable. Major research institutions and tech companies are investing heavily in the field, and collaborations between biologists, computer scientists, and clinicians are yielding increasingly sophisticated models. Some experts predict that within the next decade, digital twins could account for a significant portion of preclinical testing, drastically reducing the need for traditional trials. This shift would not only streamline drug development but also open new avenues for personalized medicine, where treatments are tailored to an individual’s unique biology.
The societal implications of this transition are profound. If digital twins can reliably replace even a fraction of human trials, the ethical landscape of medical research will be transformed. Fewer animals would be subjected to testing, and human volunteers would face fewer risks. At the same time, the democratization of medical research could accelerate, as virtual models enable smaller labs and developing countries to participate in cutting-edge studies without the need for expensive infrastructure.
Yet, for all its promise, the technology is not a panacea. Virtual organs are tools, not replacements for the complexity of living systems. They will likely serve as complements to—rather than substitutes for—traditional research methods in the foreseeable future. The key to success lies in integrating these models thoughtfully, ensuring they enhance rather than overshadow the irreplaceable value of human insight and clinical experience.
As the line between the physical and virtual worlds continues to blur, the rise of digital twins in medicine invites us to reimagine the future of healthcare. From accelerating drug discovery to enabling bespoke treatments, the possibilities are as vast as they are inspiring. But as with any transformative technology, the journey will require careful navigation—balancing ambition with caution, innovation with responsibility, and the virtual with the very real human lives at stake.
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025
By /Jul 3, 2025

By /Jul 3, 2025

By /Jul 3, 2025
By /Jul 3, 2025